If you’re considering or have been recommended for an intra-articular knee joint injection, you may have many questions and some concerns. Understanding the procedure can help alleviate any anxiety and make you feel more comfortable and confident about your treatment. This article is designed to provide you with a comprehensive guide to knee joint injections, focusing on what you can expect, how to prepare, and what happens during and after the procedure.
Intra-articular knee joint injections are a common treatment for conditions like osteoarthritis, rheumatoid arthritis, and various knee injuries. These injections can help reduce pain, improve mobility, and enhance your overall quality of life. By familiarizing yourself with the process, you’ll be better equipped to understand your treatment plan and actively participate in your healthcare decisions.
Our goal is to ensure you have the information you need to feel prepared and confident about your knee joint injection. By the end of this article, you’ll have a clear understanding of the procedure and its techniques, what to expect during your visit, and how to take care of yourself afterward.

Commonly Used Medications for Knee Joint Injections
Intra-articular knee injections involve the administration of medications directly into the knee joint to provide relief from pain and inflammation. The most commonly used medications are corticosteroids, hyaluronic acid, and platelet-rich plasma (PRP). Each of these medications works in a unique way and is indicated for specific conditions. Let’s explore how these treatments work and when they are typically used.
Corticosteroids
How They Work: Corticosteroids are powerful anti-inflammatory medications that help reduce inflammation and pain in the knee joint. When injected directly into the joint, they can quickly reduce swelling and improve mobility.
Indications:
- Osteoarthritis: Joint steroid injections are commonly used to relieve pain and inflammation in patients with osteoarthritis.
- Rheumatoid Arthritis: These injections can also be effective for managing flare-ups in rheumatoid arthritis.
- Bursitis and Tendinitis: Corticosteroids can help alleviate pain and inflammation associated with bursitis and tendinitis around the knee.
Duration of Relief: Corticosteroid injections typically provide relief for several weeks to a few months. However, they are generally not used frequently due to potential side effects with repeated use, such as joint damage or weakening of tendons.
Hyaluronic Acid
How It Works: Hyaluronic acid is a naturally occurring substance in the synovial fluid of joints that acts as a lubricant and shock absorber. Injections of hyaluronic acid aim to restore the natural viscoelastic properties of the joints fluid, which can be diminished in conditions like osteoarthritis.
Indications:
- Osteoarthritis: Hyaluronic acid injections are primarily used to treat osteoarthritis, especially in cases where other treatments have not provided sufficient relief.
- Lubrication and Shock Absorption: These injections are beneficial for patients who need improved joint lubrication and cushioning.
Duration of Relief: Hyaluronic acid injections may provide relief for several months, with some patients experiencing benefits for up to six months. The effectiveness can vary, and a series of injections might be required to achieve the best results.
Platelet-Rich Plasma (PRP)
How It Works: PRP is derived from the patient’s own blood. The blood is processed to concentrate the platelets, which are rich in growth factors that promote healing and tissue repair. When injected into the knee joint, PRP can help reduce inflammation, promote cartilage repair, and accelerate the healing process.
Indications:
- Osteoarthritis: PRP is used to treat osteoarthritis by stimulating the repair of damaged cartilage and reducing pain.
- Knee Injuries: PRP injections can also be beneficial for treating various knee injuries, such as ligament or meniscus tears.
- Tissue Healing and Regeneration: PRP is indicated for patients looking for a treatment that supports natural healing and regeneration.
Duration of Relief: PRP injections may take a few weeks to show noticeable improvement, but the benefits can last for several months to over a year. Multiple injections might be necessary depending on the severity of the condition and the patient’s response to treatment.
Summary
Each type of knee joint injection — corticosteroids, hyaluronic acid, and PRP—offers unique benefits and is suited to different conditions. Understanding how these medications work and their specific indications can help you and your healthcare provider choose the most appropriate treatment for your knee condition. Always discuss with your doctor to determine which option is best for your individual needs and to develop a comprehensive treatment plan tailored to your situation.
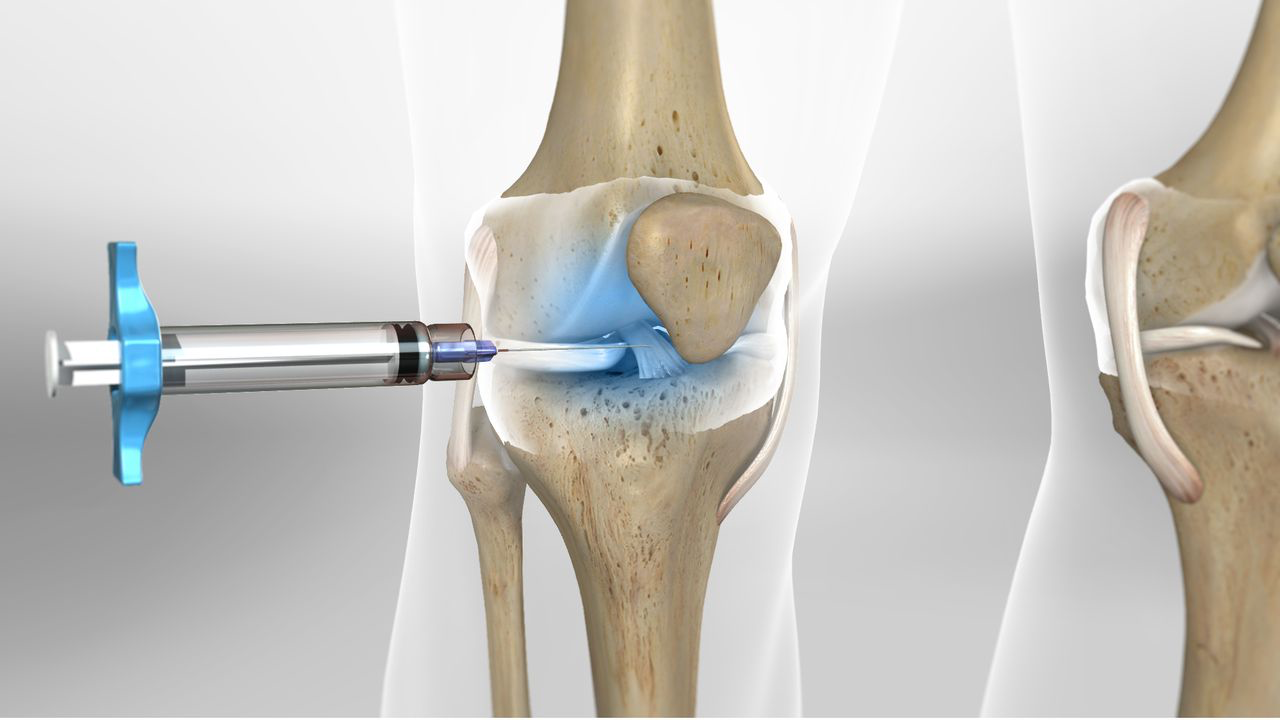
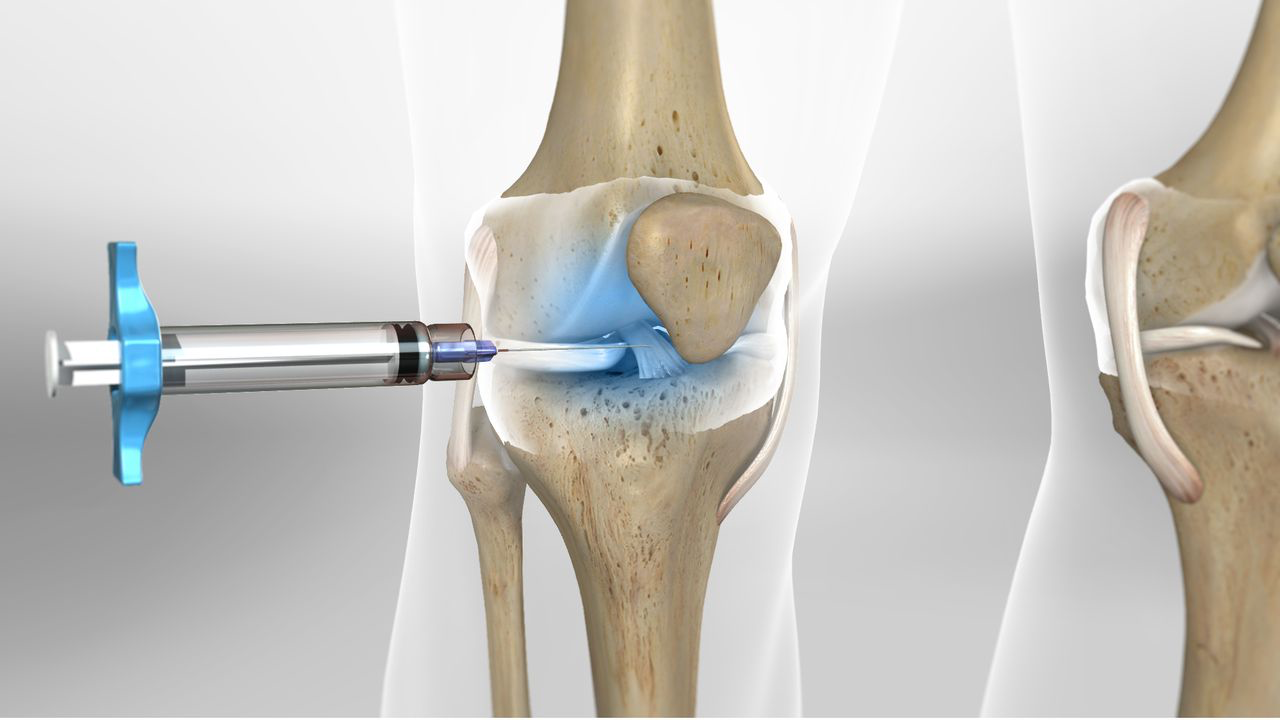
Knee Joint Injection Process Explained
Understanding the process can help ease any anxiety you may have and prepare you for what to expect during the procedure. Here is a detailed explanation of each step involved in the intraarticular joint injection process, from preparation to post-injection care.
Preparation for the Knee Injection Procedure
- Patient Assessment: Before the procedure, your doctor will review your medical history and perform a physical examination of your knee. This assessment helps determine if a knee injection is appropriate for your condition.
- Informed Consent: Your doctor will explain the procedure, including its benefits, risks, and any potential side effects. You will have the opportunity to ask questions and discuss any concerns. Once you understand the procedure, you will be asked to sign a consent form.
- Equipment and Medication: The doctor will prepare the necessary equipment, including:
- A sterile syringe and needle
- Antiseptic solution for cleaning the knee injection sites
- The chosen medication (corticosteroid, hyaluronic acid, or PRP)
The Injection Procedure
- Patient Positioning: You will be positioned comfortably on an examination table, usually lying down with your knee slightly bent. Proper positioning helps ensure the accuracy of the injection and minimizes discomfort.
- Aseptic Technique: To prevent infection, the skin around the injection site will be thoroughly cleaned with an antiseptic solution. The area will be allowed to dry before proceeding.
- Injection Site Identification: The doctor will identify the precise location for the injection. This is typically done using anatomy landmarks on the knee. In some cases, ultrasound guidance may be used to enhance accuracy.
- Numbing the Area (Optional): In some cases, a local anesthetic may be applied to the skin to numb the area and minimize discomfort during the injection.
- Administering the Injection:
- The doctor will carefully insert the needle into the knee joint. You may feel a slight pinch or pressure.
- Once the needle is in place, the medication will be injected slowly into the joint.
- The needle is then removed, and the injection site may be covered with a small bandage.
Post-Injection Care
- Immediate Aftercare. After the injection, you will be asked to rest for a few minutes. The doctor will monitor you for any immediate reactions.
- Activity Restrictions. You will receive specific instructions about activities to avoid post-injection. Generally, you should avoid strenuous activities and heavy lifting for at least 24 to 48 hours. Gentle movement and normal daily activities are usually encouraged to help distribute the medication within the joint.
- Managing Discomfort. It is common to experience mild discomfort or swelling at the injection site for a day or two. Applying an ice pack to the area can help reduce swelling and alleviate pain. Over-the-counter pain relievers, such as acetaminophen, can also be used if needed.
- Signs of Complications. Your doctor will inform you of potential signs of complications, such as increased pain, swelling, redness, or fever. If you experience any of these symptoms, contact your healthcare provider immediately.
- Follow-Up Appointments. A follow-up appointment may be scheduled to assess the effectiveness of the injection and discuss further treatment options if needed. Your doctor will also evaluate your progress and address any concerns you may have.
Contraindications, Potential Risks and Complications and Ways to Avoid Them
While knee joint injections are generally safe and effective, it’s important to be aware of contraindications, potential risks, and complications. Understanding these factors can help you make an informed decision and take steps to minimize any risks.

Contraindications
There are certain conditions and situations where intra-articular joint injections may not be recommended. These contraindications include:
- Active Infection. If there is an active infection in the knee or elsewhere in the body, injecting into joints could potentially worsen the infection.
- Bleeding Disorders. Patients with bleeding disorders or those taking blood thinners may have an increased risk of bleeding or bruising at the injection site.
- Allergy to Medication. If you have a known allergy to the medication being used (e.g., corticosteroids, hyaluronic acid), the injection should be avoided.
- Severe Osteoarthritis. In cases of advanced osteoarthritis where the joint space is severely narrowed, the effectiveness of injections may be limited.
- Uncontrolled Diabetes. High blood sugar levels can increase the risk of infection and may be temporarily affected by corticosteroid injections.
- Skin Problems. Skin conditions such as psoriasis or eczema at the injection site can increase the risk of infection.
Potential Risks and Complications
Even though intra-articular joints injections are minimally invasive, there are potential risks and complications, including:
- Infection. Although rare, there is a risk of infection at the injection site. Signs of infection include increased redness, swelling, warmth, and fever.
- Pain and Swelling. Some patients may experience temporary pain and swelling at the injection site. This is usually mild and resolves within a few days.
- Allergic Reactions. Allergic reactions to the injected medication are uncommon but can occur. Symptoms may include rash, itching, and difficulty breathing.
- Bleeding or Bruising. Minor bleeding or bruising at the injection site can happen, especially in patients with bleeding disorders or those on blood thinners.
- Nerve or Tissue Damage. In rare cases, the needle may cause damage to surrounding nerves or tissues.
- Steroid Flare. Corticosteroid injections can sometimes cause a “flare” of pain and inflammation in joints shortly after the injection, lasting for a day or two.
- Joint Instability. Repeated corticosteroid injections can potentially weaken tendons and ligaments, leading to joint instability over time.
Ways to Avoid Risks and Complications
To minimize the risks and complications associated with knee joint injections, follow these guidelines:
- Choose an Experienced Practitioner. Ensure that the procedure is performed by a qualified and experienced healthcare provider who is familiar with the intra articular knee injection technique.
- Discuss Your Medical History. Provide your doctor with a complete medical history, including any allergies, current medications, and underlying health conditions.
- Follow Pre-Procedure Instructions. Adhere to any pre-procedure instructions given by your doctor, such as fasting or adjusting medications.
- Maintain a Sterile Environment. The injection should be performed in a clean, sterile environment to reduce the risk of infection.
- Monitor for Signs of Complications. After the injection, keep an eye on the injection site and overall symptoms. Report any signs of infection, severe pain, or unusual reactions to your doctor immediately.
- Limit Activities Post-Injection. Follow your doctor’s advice on activity restrictions after the injection to avoid putting undue stress on the knee joint.
- Schedule Follow-Up Appointments. Attend any scheduled follow-up appointments to monitor the effectiveness of the injection and address any issues early.
By understanding the contraindications, potential risks, and complications associated with intra-articular knee joint injections, and taking steps to avoid them, you can ensure a safer and more effective treatment experience. Always communicate openly with your healthcare provider and follow their recommendations for the best possible outcomes.
Frequently Asked Questions & Common Patient Concerns
Here, we address some of the most frequently asked questions and common concerns patients have to help you feel more informed and comfortable about the procedure.
1. How long does the injection procedure take?
The actual injection process typically takes only a few minutes. However, including preparation and post-injection monitoring, you can expect the entire visit to take about 30 to 45 minutes.
2. Will the injection hurt?
Most patients experience only mild discomfort during the injection. A local anesthetic may be used to numb the area, reducing any pain. You might feel a slight pinch or pressure when the needle is inserted.
3. How soon will I feel relief after the injection?
Relief times can vary depending on the type of medication used. Corticosteroids often provide relief within a few days, while hyaluronic acid and PRP may take several weeks to show significant improvement.
4. How long will the effects of the injection last?
The duration of relief varies. Corticosteroid injections can last from several weeks to a few months. Hyaluronic acid may provide relief for several months, and PRP can offer benefits for six months or longer.
5. How many injections will I need?
The number of intraarticular injections required depends on your specific condition and how you respond to treatment. Some patients achieve sufficient relief with a single injection, while others may need a series of injections.
6. Are there any activity restrictions after the injection?
Yes, you should avoid strenuous activities and heavy lifting for 24 to 48 hours after the injection. Light activities and normal daily movements are usually fine and can help distribute the medication in the joint.
Intra-articular knee joint injections are a valuable treatment option for managing various knee conditions, providing significant relief from pain and improving mobility. This comprehensive guide has aimed to demystify the process for patients, helping you understand the purpose, procedure, potential risks, and benefits of knee joint injections.
Ultimately, knee joint injections can be a highly effective way to manage knee pain and enhance your quality of life. By partnering with your healthcare provider, following their recommendations, and staying informed, you can confidently navigate your treatment journey and look forward to better joint health and mobility. If you have any further questions or concerns, don’t hesitate to reach out to your medical team—they are there to support you every step of the way.


